What’s an OT?
As a caregiver and patient, you encounter various healthcare professionals when experiencing medical events, health concerns, or even when you or your child are healthy. There are physicians, physical therapists, behavioral therapists, speech therapists, and our personal favorite- occupational therapists. But what is an occupational therapist?
Occupational Therapist
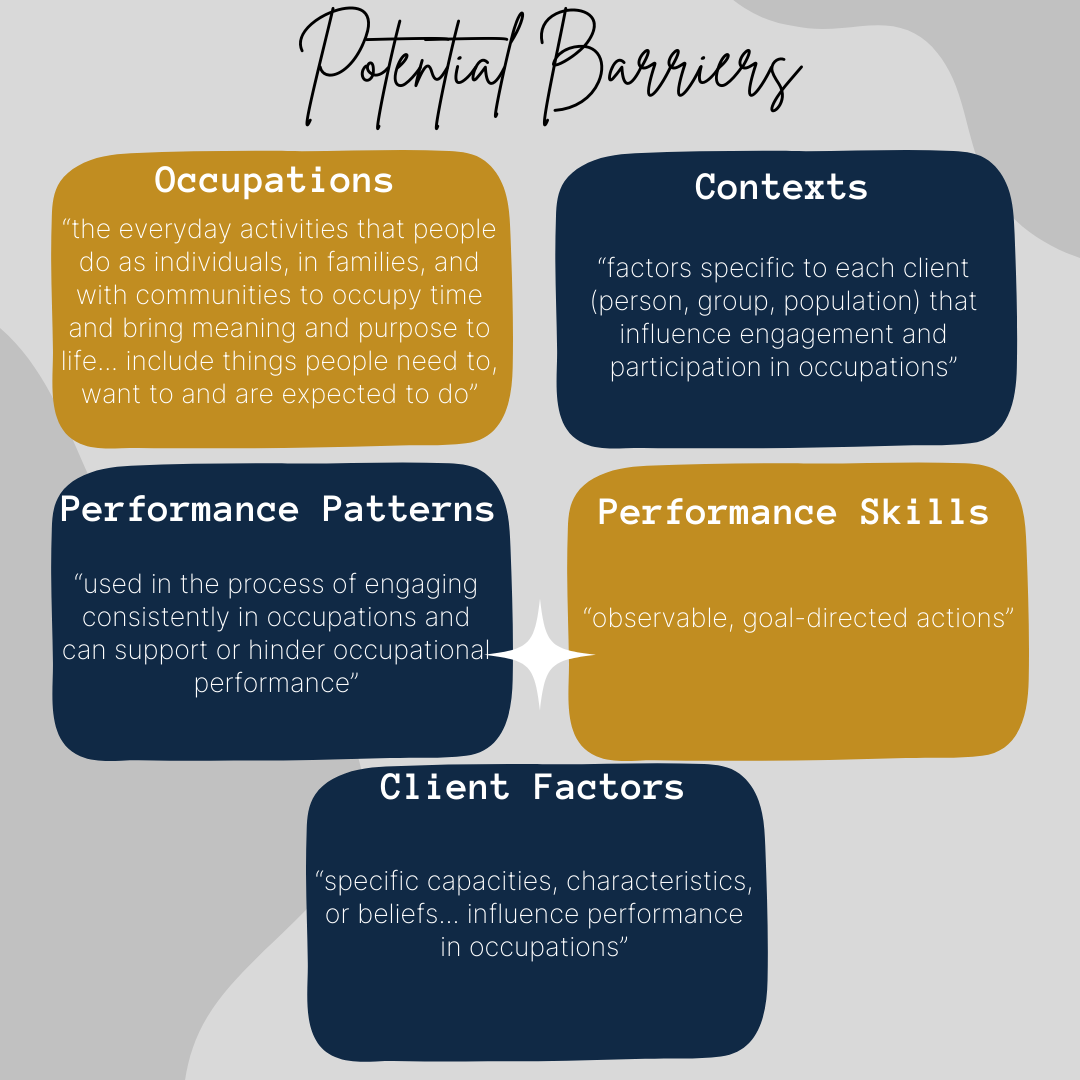
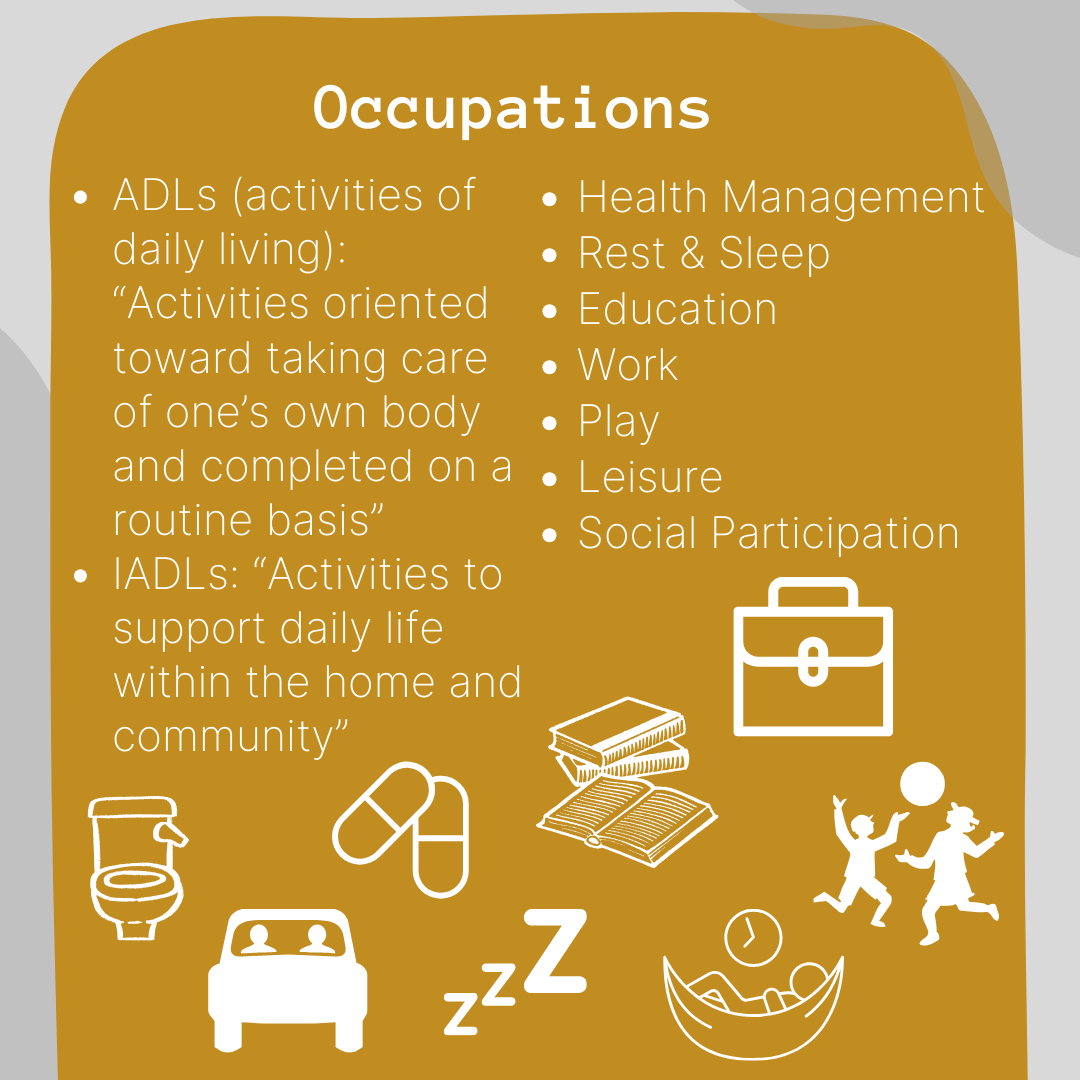
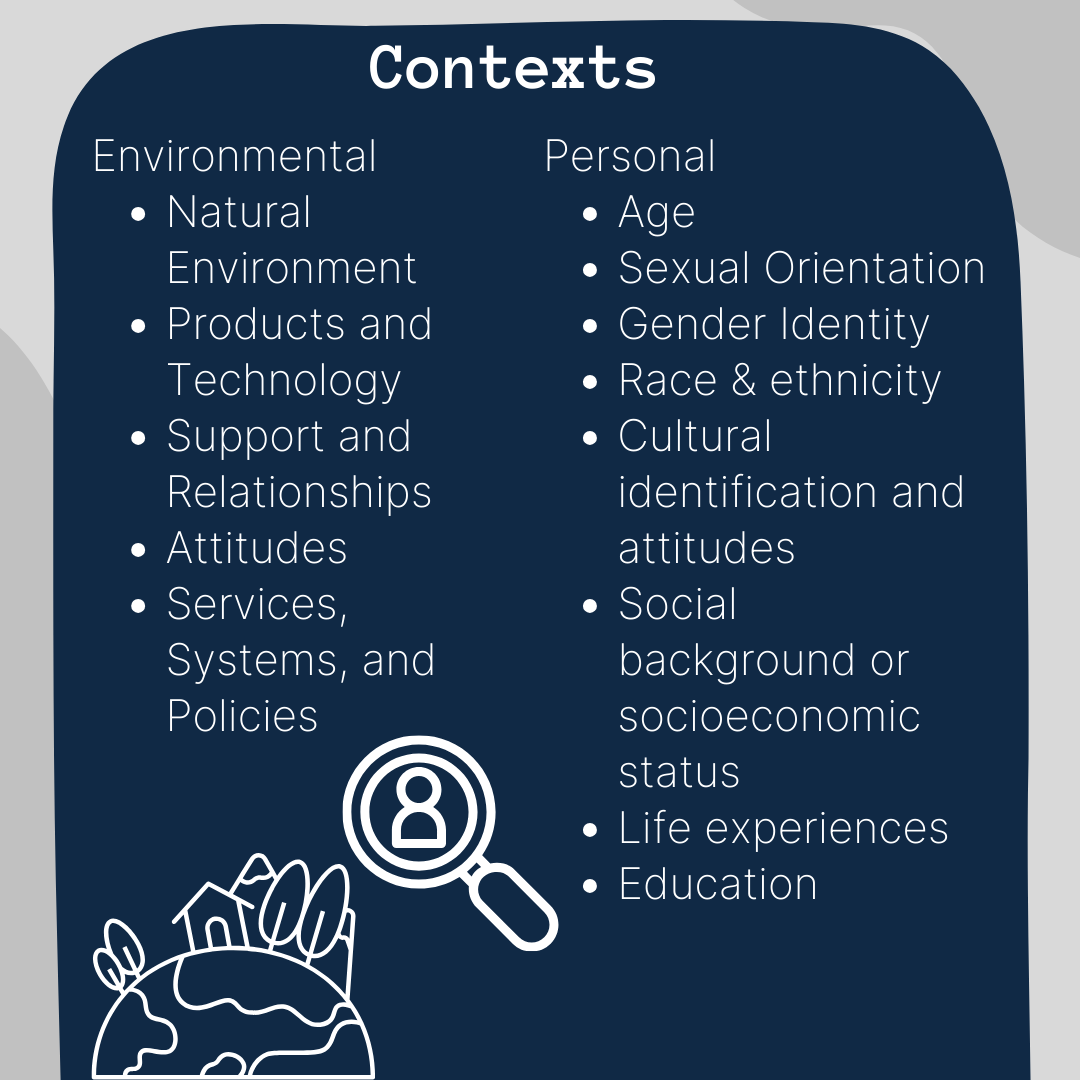
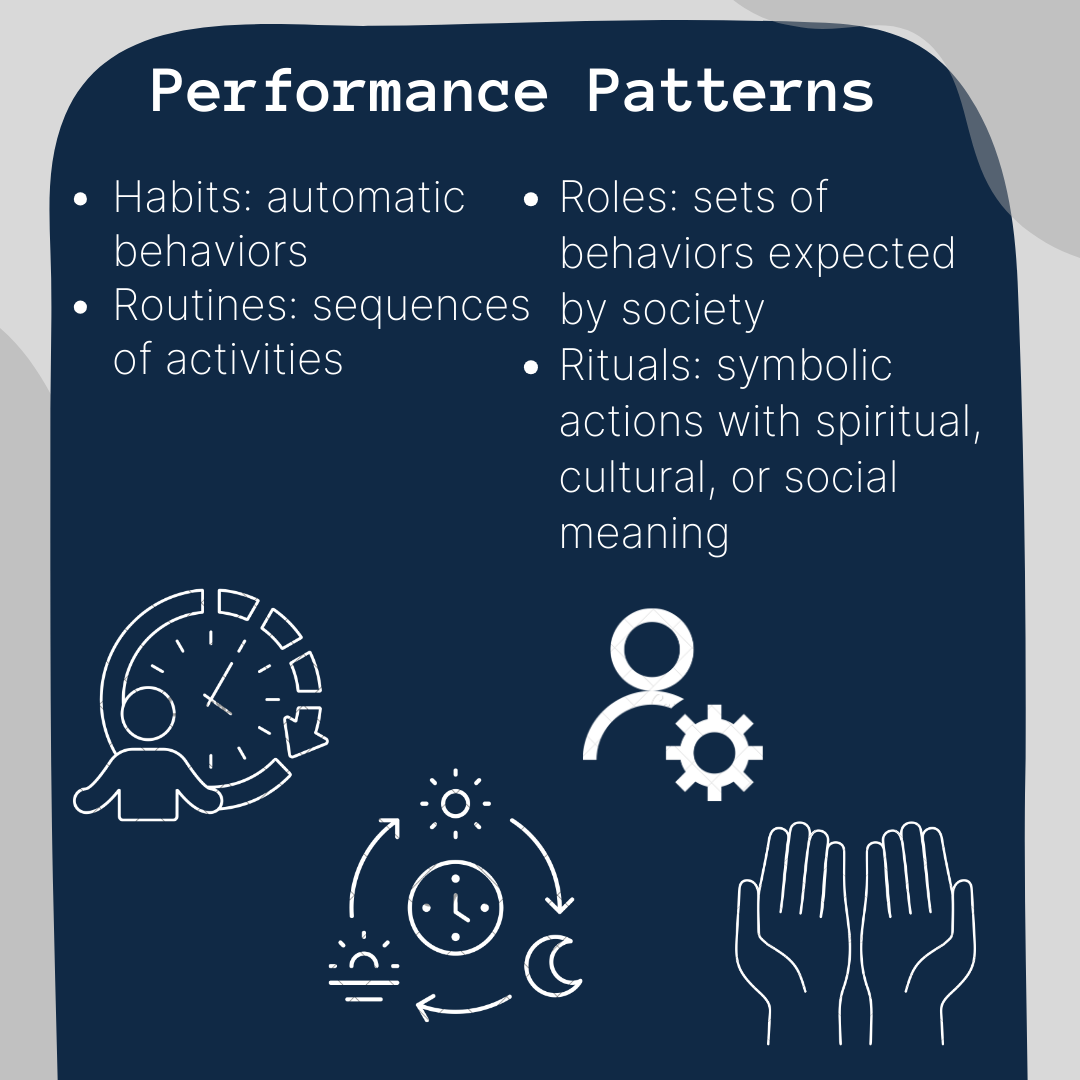
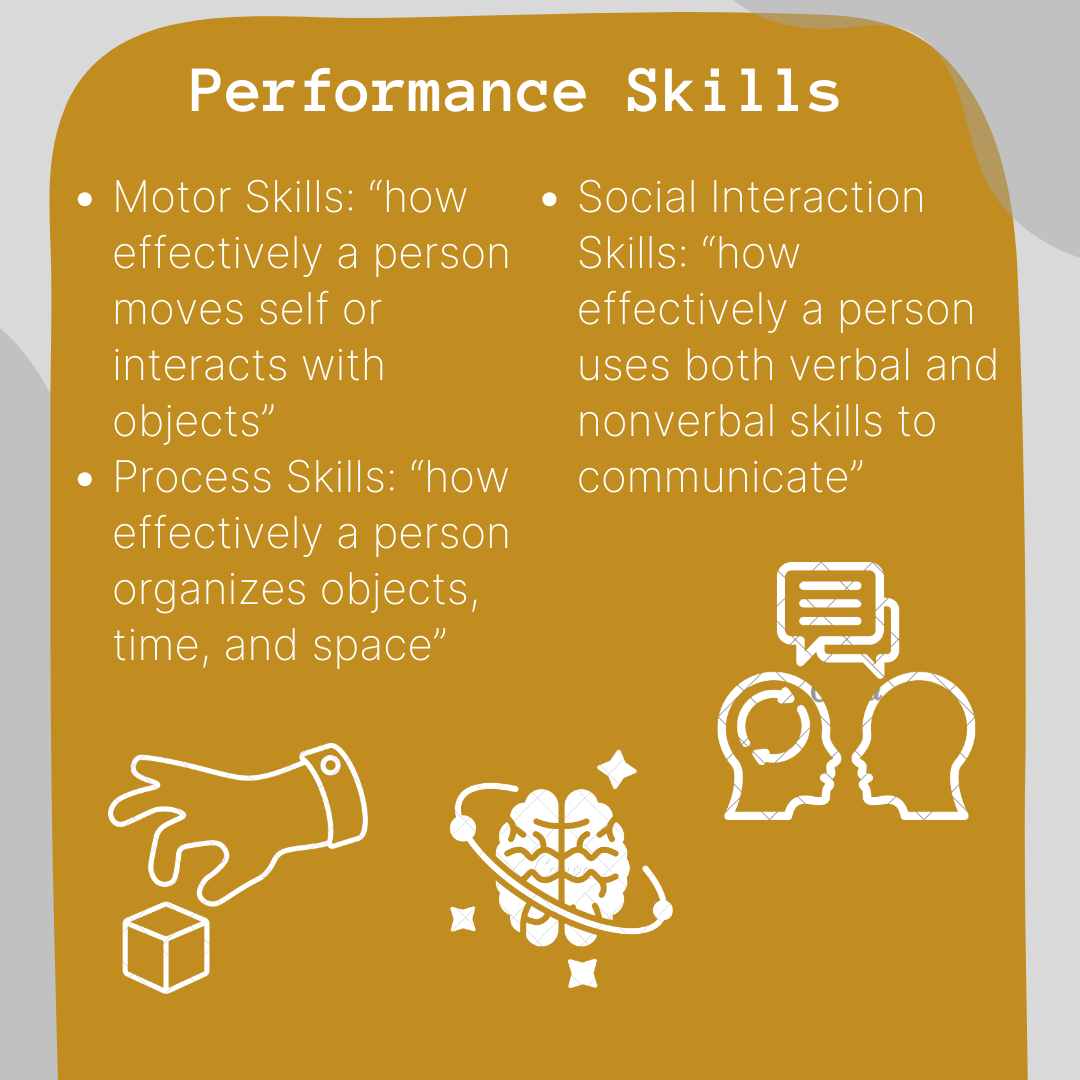
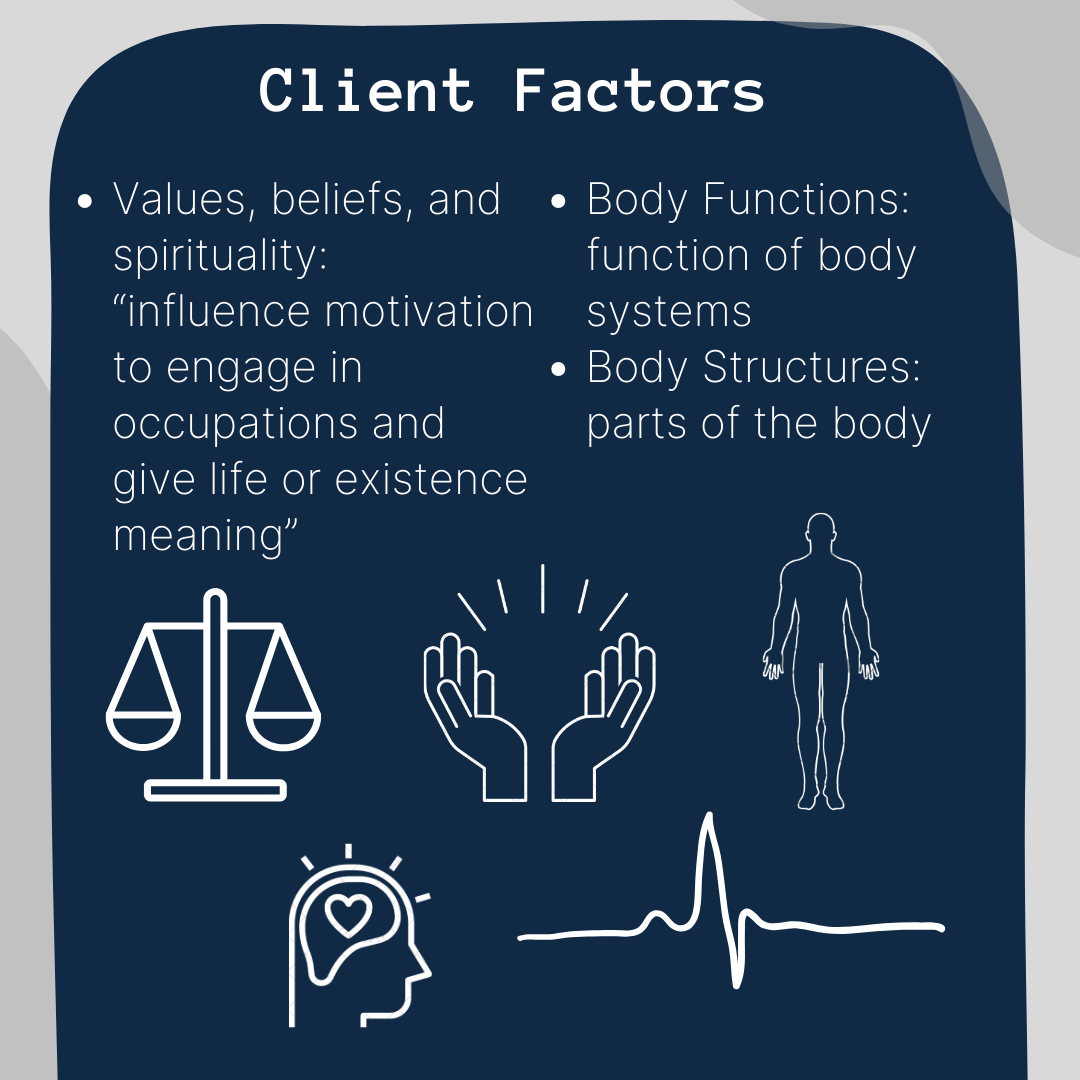
The name may be confusing- we don’t help people find jobs! Occupational therapists, otherwise known as OTs, help their clients return to doing the activities they want to do or need to do, but are unable to due to activity or contextual barriers, performance patterns, performance skills, or other client factors (American Occupational Therapy Association [AOTA], 2020). A more detailed explanation of the barriers are shown below. A referral may occur or a family may seek out OT services when there are concerns about general performance with motor skills or cognitive ability, inability to complete daily tasks, decreased strength or endurance, delays in common milestones, or difficulty with emotional regulation.
The Process
The Initial Evaluation
OTs help their clients with barriers through a standard but complex process. We begin with a consultation and evaluation of the client, often including a review of their history, a consultation, and formal/informal assessments. Evaluations are essential for finding out what daily tasks a client wants or needs to do, previous daily activities, and where or from whom they receive support. One of the most common tools we use is the occupational profile, which summarizes the above barriers someone may experience. This information is often gathered through an interview or observation of the client. Observations also help OTs analyze someone’s ability to perform daily activities before their very eyes. In an outpatient setting, this can take anywhere from 30 minutes to an hour, but observations can also occur at school, at home, or anywhere there is a concern about activity performance. OTs also typically use assessments, of which there are TONS. In children, they can assess language, fine-motor, gross-motor, self-help, cognitive, visual, handwriting, sensory-processing, and social-emotional skills to name just a few. This helps determine whether your child is experiencing challenges with the physical, emotional, cognitive, and/or social domain, and often where they may need the most help at school. Prior to receiving an assessment, there should be consistent data or observations from parents, teachers, or physicians about concerns regarding the child. Typically a child has to fall at least two standard deviations from the norm (average score) in at least one area of an assessment to qualify for OT services, but this can also be at the discretion of the OT.
The Intervention
Next comes intervention- this is when we work with clients so they can reach their goals. In OT we tend to have short-term goals (to be completed within a few weeks) and long-term goals (to be completed within months), and they are typically pretty specific. Below are a few examples
Client will demonstrate increased core strength from 3/5/24 to 4/5/24 by creeping 15 feet to obtain toy for play by end of the month.
Client will be able to hold a pencil with a developmentally appropriate grasp and write their name independently with 80% accuracy in ⅘ trials by 5/24/24.
Client will share an item with their sibling for 1 minute, without aversion, in ⅘ trials by 12/15/24.
Interventions vary widely as every barrier and every client is different. Interventions can differ based on client goals, health, performance, environment, and evidence on what works best. Different types of interventions include performing occupations or activities, providing bodily supports like a wheelchair, cast, or technology, providing education or training, and advocating for clients. Not only are there different interventions, there are also numerous approaches to interventions, including promoting health, remediating skills or abilities, maintaining skills or abilities, modifying activities, and preventing disabilities. This is why OT interventions look so different from client to client and how OTs work with anyone from infancy to older adults. For pediatric OT, this often looks like play because, believe it or not, many of our foundational skills originate in play. When your child spins or climbs they are working on activating their sensory systems, when they play catch they are working on sensory and perceptual-motor development, and when we share our toys we work on cognitive intellect.
The Outcomes
Finally, there are the outcomes. Outcomes describe the client’s results achieved through the OT process. These outcomes include the ability, improvement, and/or increased participation in an activity, prevention of unhealthy conditions, increased health and wellness/well-being/quality of life, ability to partake in a role, or increased access to meaningful activities. This is what we, occupational therapists, work to achieve with clients through our interventions. This process can be anywhere from weeks to years depending on the person or circumstances. Similarly, you can see an OT anywhere from daily to weekly to monthly, again depending on needs and severity. Sometimes, especially with children, a therapeutic break is also an option. A full pause from OT services can be beneficial, as it allows you to gain some perspective on your growth and goal progress, work on transferring skills from the clinic to the hospital or home setting consistently, and take an overall rest. This is something your OT may even suggest when it seems your child is beginning to feel frustrated, lack motivation during sessions, or hit a plateau. OT is hard work! This should be a collaborative decision and should not occur suddenly or unexpectedly. There are also transfers of care in which a client will move from a hospital to a clinic, clinic to home, or hospital to home. These changes can be scary for a child, but they are important for continued progression. Your child will likely get a new OT, one who has become knowledgeable on their case and progress and is working towards the same goals as you, your child, and the previous OT. This is a great time to inform the new OT about what your child likes, dislikes, and what has worked great at sessions in the past. Be their advocate!
Where do they work? And who do they work with?
OTs can work almost anywhere and everywhere. We can work with older adults or those with mental health diagnoses who live in long-term care facilities, with stroke or traumatic brain injury patients in hospitals, with kids in schools, homes for those who have barriers to leaving the house, and in clinics doing everything in-between. Where there are people, there are OTs!
It’s a tricky question to answer, “who do we work with”. That’s because it can be anyone! OTs provide services to anyone from birth to end-of-life, those with physical, mental, or cognitive disabilities, private and federal insurance, you name it! That is the beauty of OT, no matter who you are, we strive to help you become the best version of yourself. For us, it is not always about doing it the way it’s always been done but doing it in a way that works for YOU. If you can function with a new condition as you were before, then OT is likely not needed! When you start to see the effects of a disability or a diagnosis in your life, that’s when we come into play. As long as we can ensure you are able to do what you want and need to do- that’s all that matters.
So, how can I see an OT?
To see an occupational therapist, you will need to be referred, typically by your physician. In most states and through most insurances, this is a requirement. If you think you or someone you love would benefit from OT, talk to your physician. You may be able to receive a screening or evaluation without a referral, but in order to proceed with interventions, it would be necessary (Shane, n.d.). Additionally, if you think your child would benefit from receiving OT in school, then talk about it in their Individualized Education Program (IEP) meeting. If you don’t have this again, you can talk to your child’s physician, or talk with your social worker. If you don’t have a social worker you can look into getting one through the Minnesota Department of Human Services. In Minnesota, a physician referral is not required for school-based OT, but is instead up to the Special Education team (Minnesota Department of Human Services [MNDHS], 2023). The IEP process can take time and requires extensive data, so being proactive and advocating for your child is vital.
Whoever you are and whatever you are trying to accomplish, we are here to help!
References
American Occupational Therapy Association. (2020). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy, 74(Suppl. 2), 7412410010. https://doi.org/10.5014/ajot.2020.74S200
Children’s Minnesota. (n.d.). Occupational therapy. https://www.childrensmn.org/services/care-specialties-departments/physical-rehabilitation/occupational-therapy/#:~:text=When%20is%20an%20occupational%20therapy,care%20skills%20(dressing%2C%20grooming)
Minnesota Department of Human Services. (2023). Occupational therapy services (OT) services. https://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVERSION&RevisionSelectionMethod=LatestReleased&dDocName=DHS16_188590
Shane, S. (n.d.). OT process and the four levels of intervention. Pass The OT. https://passtheot.com/ot-process-4-levels-intervention-module-one-ota/
World Federation of Occupational Therapists. (2012a). About occupational therapy. Retrieved from https://www.wfot.org/about-occupational-therapy


